Introduction
The clinical outcome of non-transplant eligible patients with newly diagnosed Multiple Myeloma (NDMM) is heterogeneous, largely depending on frailty level. Clinical scores such as the International Myeloma Working Group frailty index (IMWG-FI) classify patients in categories ‘fit’, ‘intermediate-fit’ or ‘frail’. As disease and treatment burden can change over time, frailty can improve but also deteriorate during treatment. However, data are scarce and the effects on clinical outcome are largely unknown. To address this, we prospectively investigated the dynamics of frailty scores and impact on clinical outcome of non-transplant eligible patients with NDMM (NTE-NDMM) included in the HOVON 143 study.
Methods
The HOVON 143 study included NTE-NDMM classified as intermediate-fit (score 1) or frail (score ≥2) by the IMWG-FI (score ranging from 0 to 5, fit being defined as 0). Patients were treated with nine 28 days-cycles of ixazomib (4mg on days 1, 4, 15), daratumumab (16mg/kg iv; cycles 1-2: days 1, 8, 15, 22; cycles 3-6: days 1, 15; cycles 7-9: day 1) and low dose dexamethasone (cycle 1-2: 20mg; subsequent cycles 10mg, co-administered with daratumumab). The IMWG-FI was calculated at baseline, after 3 and 9 cycles. A joint model was employed to model survival outcomes and longitudinal frailty score data. For this purpose, a cox model was used to model survival outcome and a mixed-effects model to model longitudinal frailty score data (R statistical program, package JM).
Results
Of the 130 included patients, 65 were intermediate-fit at baseline and 65 patients were frail (49% score 2, 28% score 3, 22 % score 4, 1% score 5). After nine cycles, 82 patients were still on protocol of whom frailty level over time was known in 74 patients (39 intermediate-fit, 35 frail).
Six/35 frail patients could not improve in frailty score as well as category, as they were classified as ‘frail’ due to age >80 years without any impairments or comorbidities. Of the 29 frail patients that could improve, 14 (48%) improved in frailty score. Of those, 5 patients became intermediate-fit, 1 became fit and 8 remained frail because of still having a score of ≥2. Reasons for improvement were becoming less iADL dependent (11/14), less ADL dependent (10/14), or both (8/14). Improvement in Charlson Comorbidity Index (CCI) occurred in 4/14. Six out of 34 (18%) who could deteriorate in frailty score (excluding the patient with frailty score of 5), did so. Two frail patients became ADL dependent, 2 became iADL dependent and 2 deteriorated in score solely due to age (turning 81 years old during treatment).
Out of the 39 intermediate-fit patients that could improve in frailty score, 6 (15%) improved and consequently became fit (frailty score from 1 to 0). Reasons for improvement were becoming less ADL dependent (3/6) and improved CCI (3/6). Five intermediate-fit patients (13%) deteriorated. One intermediate-fit patient became iADL dependent (1/5), 1 patient acquired a comorbidity (1/5) and 3 deteriorated in score solely due to age (turning 76 old during treatment).
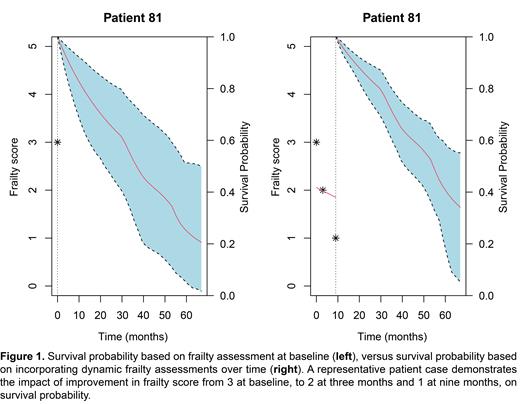
Median duration of follow up of all 130 patients was 46 months. Including frailty score as a time varying covariate in survival analysis by a joint model indicated that the frailty score improved over course of treatment, and that improvement of frailty score was associated with higher survival probabilities (HR 0.58 (95%CI 0.42 - 0.79), p<0.001) ( Figure 1).
Conclusion
This is the first study to report the dynamics in IMWG frailty assessment of non-transplant eligible patients with NDMM during a clinical trial. The frailty score improved in nearly half of frail patients and 15% of the intermediate fit patients during MM treatment. This led to reclassification to intermediate-fit or fit in a substantial number of patients. Improvement of the frailty score was associated with prolonged survival. Future studies are needed to investigate whether dynamic frailty status is a better predictor for clinical outcome than frailty status at baseline.
Disclosures
Stege:Sanofi: Consultancy, Speakers Bureau; Celgene/Bristol Myers Squibb: Speakers Bureau; Takeda: Speakers Bureau; Janssen: Consultancy. Van Der Spek:Janssen: Honoraria, Other: Payment or honoraria for lectures, presentations, manuscript writing or educational events. Nijhof:Janssen: Honoraria, Speakers Bureau; Celgene/Bristol Myers Squibb: Honoraria, Speakers Bureau; Sanofi: Honoraria, Speakers Bureau. Kentos:Janssen-Cilag: Consultancy; Amgen: Consultancy; Sanofi: Consultancy. Timmers:Novartis: Consultancy, Other: Travels, accomodations, expenses; Janssen: Other: Travels, accomodations, expenses. Vekemans:Menarini: Consultancy; GlaxoSmithKline: Consultancy; Pfizer: Consultancy; Amgen: Consultancy, Honoraria, Other: Payment or honoraria for lectures, presentations, manuscript writing or educational events, Speakers Bureau; Celgene/Bristol Myers Squibb: Consultancy, Honoraria, Other: Payment or honoraria for lectures, presentations, manuscript writing or educational events, Speakers Bureau; Janssen: Consultancy, Honoraria, Other: Payment or honoraria for lectures, presentations, manuscript writing or educational events, Speakers Bureau; Takeda: Honoraria, Other: Payment or honoraria for lectures, presentations, manuscript writing or educational events, Speakers Bureau; Sanofi: Consultancy. van de Donk:BMS: Other: Advisory Board, Research Funding; Cellectis: Research Funding; Novartis: Other: Advisory Board, Research Funding; Takeda: Other: Advisory Board; Roche: Other: Advisory Board; Bayer: Other: Advisory Board; Pfizer: Other: Advisory Board; Abbvie: Other: Advisory Board; Adaptive: Other: Advisory Board; Servier: Other: Advisory Board; Celgene: Other: Advisory Board, Research Funding; Amgen: Other: Advisory Board, Research Funding; Janssen Pharmaceuticals: Other: Advisory Board, Research Funding. Ypma:Janssen: Other: support for attending meetings and/or travel; Janssen: Honoraria. Zweegman:Sanofi: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal